CHRONIC OBSTRUCTIVE PULMONARY DISEASE
CAUSES & SOLUTIONS
“Chronic obstructive pulmonary disease is a leading cause of morbidity and mortality worldwide and is expected to increase as the population ages. Patients have a high symptom burden and low healthcare quality of life.” From this month’s issue of Current Opinion in Pulmonary Medicine
“Gray matter [brain] volume deficits have been identified in cognitively impaired patients with chronic obstructive pulmonary disease (COPD). The present study confirmed that brain structural changes were present in stable COPD patients with subclinical [minimal / invisible] cognitive impairment.” From this month’s issue of Neurotoxicity Research
“Aging is a progressive degeneration of the tissues that has a negative impact on the structure and function of vital organs. Many of the changes that occur in the lungs with normal aging, such as decline in lung function, increased gas trapping, loss of lung elastic recoil, and enlargement of the distal air spaces, also are present in chronic obstructive pulmonary disease (COPD). COPD has been considered a condition of accelerated lung aging. Increasing age leads to elevated basal levels of inflammation and oxidative stress (inflammaging)……” From this month’s issue of the Annals of the American Thoracic Society
COPD stands for Chronic Obstructive Pulmonary Disease, and as you can begin to see from the quotes above, it’s a serious problem that can affect sufferers in any number of different ways. The term “COPD” encompasses several diseases, but has a specific cluster of pathologies that makes it unique.
- COPD IS INFLAMMATORY: C-Reactive Protein (CRP) is one of the best blood markers of inflammation. A brand new study from the International Journal of COPD (COPD Assessment Test Score and Serum C-Reactive Protein Levels…) revealed that, “In stable COPD patients, serum CRP levels were independently associated with total CAT score and CAT components [both measurements of COPD] related to respiratory symptoms, confidence leaving home, and energy.” Inflammation is a group of chemical compounds manufactured by your immune system in response to tissue damage (please note that said tissue damage can occur in any number of ways — HERE are the three main categories). The inflammatory mediators mentioned in several COPD studies include many I’ve talked about on my site (HERE), TNF-α, IFN-γ, MMP-6, MMP-9, CRP, IL-1, IL-6, IL-8, and others. Not only do these dramatically diminish the size of the airway via swelling, but even worse, they diminish it chronically as inflammation always leads to increased fibroblastic activity, ramped up fibrinogen production, and eventually something called “Fibrosis,” which happens to be the leading cause of death in America (HERE). Because the last quote below the pic above mentions OXIDATIVE STRESS, it’s important for you to grasp this concept as well since it is related (HERE also).
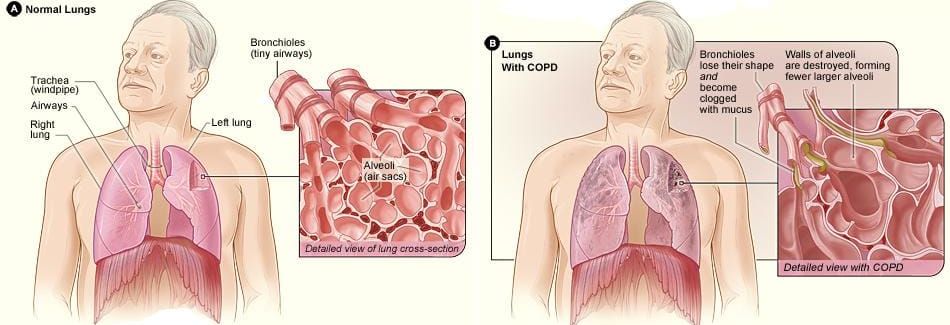
- PARENCHYMAL DESTRUCTION: Parenchyma is a rather vague term used to describe the functional part of a tissue or organ as opposed to its structural portion. It is this feature of COPD that is said to make breathing so difficult. Although it might not feel this way, people with COPD can get lots of air into their lungs; they can’t get it out. The alveolar sacs in the lungs, where O2 is exchanged for CO2 and vice versa, lose their ability to stretch and elast, kind of like a balloon that has been repeatedly over-inflated. Over time they lose their elasticity, which hinders the ability to push air out. Furthermore the lung’s smaller airways actually collapse on themselves when a person with COPD exhales. These two factors leave an abnormal amount of air trapped in the lungs in perpetuity. I’ve heard people describe breathing with COPD as taking the biggest breath you could possibly take, and then breathing through a straw (try it, but make sure to pinch your nose). This excessive amount of residual air in the lungs constantly pushes outward, frequently causing the characteristic signature of COPD — particularly emphesyma — a humped back and pigeon breast.
- INCREASED MUCOUS PRODUCTION & CHRONIC COUGH: The cells on the inside surface of the airways are covered with cilia; tiny hair-like filaments that wave back and forth helping to move solid particulate matter and mucous out of the lungs and into the throat, where it can either be swallowed or expelled (spit out). Due to any number of factors (chiefly smoking), not only are the cilia damaged / destroyed, but the cells themselves can be damaged to the point they must be replaced. The body tends to replace these with goblet cells (goblet cells secrete “gobs” of mucous). As you might imagine, this is yet another way that airflow is compromised, leading people to paroxysmal coughing fits as they try to expel this junk from their shrinking airways. This feature of COPD is usually referred to by the medical community as “Chronic Bronchitis”.
Ultimately, these folks can’t breathe and are left to the treatments prescribed by their physicians. The first line of defense are the bronchodilators commonly used to treat people with ASTHMA. Because asthma is not considered one of the diseases that makes up COPD, these are not very effective. Next comes CORTICOSTEROIDS, which work by suppressing the immune system, thereby suppressing inflammation. While these drugs certainly work on some level, their effects are short-lived and they have many harsh side-effects, including OSTEOPOROSIS. This is especially problematic for individuals already dealing with COPD-associated hyper-kyphosis (humpback).
It goes without saying that folks with COPD end up on oxygen, with many having surgery. Because hyper-inflation is the common denominator with COPD, the most common surgery involves removing stretched out lung tissue, which makes it more difficult for the lungs to become over-inflated. Some even get lung transplants, which create their own unique set of problems (survival rate is about 50% at five years). The real question that most of you need to be asking is whether or not there is anything you, the suffering patient, could be doing to help yourself beyond standard medical fare?
- EXERCISES: Let me start by saying that most people with COPD are to at least some degree, exercise intolerant. I am not talking here about intolerance to things like running two or three miles, but walking down the hall. There are any number of YouTube Videos loaded with fantastic information about specific breathing exercises — DIY respiratory therapy if you will. Beyond that, regular physical exercise has been shown by research to be extremely beneficial for people with COPD and should be done to tolerance (make sure to add some sort of strength regimen to counteract the steroids — HERE). I am a huge fan of things like Yoga and similar that will help keep the rib cage mobile (HERE’S another) . One I often recommend for people is to get a bar and hang. This is not INVERSION, but simply taking hold of something overhead and stretching your rib cage out by hanging some or all of your weight. Speaking of weight…
- MAINTAIN A NORMAL WEIGHT: Obesity is a significant factor in one’s ability (or inability as the case may be) to breathe. We see this in SLEEP APNEA as well as asthma. Obesity also happens to be, right along with COPD itself, another of the myriad of diseases caused by inflammation. This means that you need to….
- CONTROL INFLAMMATION: While this is certainly easier said than done, it may not be as difficult as you think. If you have not stopped smoking, by all means do so. And make doubly sure you deal with THIRD HAND SMOKE by giving your house a total top-to-bottom cleaning (this will help with air quality as well by dealing with known irritants such as BLACK MOLD). Beyond this, as you know I’m a stickler for the PALEO DIET because of it’s amazing ability to control inflammation. Be aware, however, that there are any number of things that can drive inflammation and any number of ways to help control it (HERE is a great general resource).
- USE THE WEB TO YOUR ADVANTAGE: As I researched this post, I saw lots and lots of interesting, non-invasive, non-pharmacological methods of addressing COPD on the internet. Use the internet to your advantage and create a written plan for addressing your problem. Just remember to work the plan.
- CHIROPRACTIC ADJUSTMENTS: Last but not least, I have to mention that for many individuals with COPD, CHIROPRACTIC ADJUSTMENTS are a godsend. Although there is certainly a neurological connection for explaining this (see link), mostly it’s because the adjustments help keep the thoracic cage from locking up so badly as it over-expands due to the constant pressure of hyper-inflated lungs. As big a fan as I am of adjustments, working your plan means you’ll need fewer of them.
If you are liking what you are seeing, be sure to like, share or follow on FACEBOOK.
