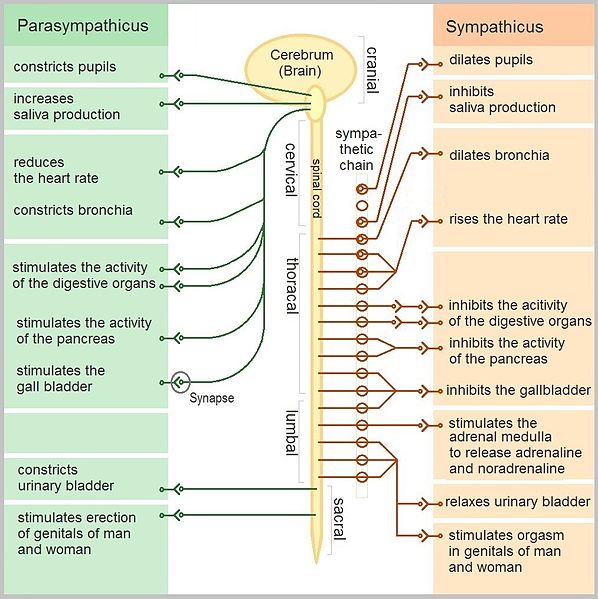
The HYPOTHALAMUS is a small part of your brain responsible for a lot of big things. Among others, it helps regulate the part of your nervous system that deals with unconscious (or “automatic”) bodily functions such as heart beat, respiration, blood pressure, and digestion known as the Autonomic Nervous System. The Autonomic Nervous System comes in two different flavors — Sympathetic and Parasympathetic.
The Sympathetic Nervous System is your “fight or flight” system, whose chief neurotransmitter is epinephrine (previously known as adrenaline). On the other side of the coin is the Parasympathetic Nervous System, which is related to rest, relaxation, and digestion. These two systems should work in tandem, creating the balanced state of being we call HOMEOSTASIS, with, as you might guess from what you’ve already learned, the parasympathetic system being the dominant system. But what happens if Parasympathetic Dominance is reversed?
Imagine for a moment that instead of the Parasympathetic Nervous System spending most of the time in the body’s driver’s seat, the Sympathetic Nervous System were running the show. Instead of a body living in a generally relaxed state; digesting well, pumping blood via low pressure, with a heart rate that only speeds up when needed, you have a body existing in a perpetually hyped state. Always hungry but never satisfied. Always exhausted but never able to sleep. Heart always racing, but unable to physically exert. Wanting to have an orgasm, but unable to become sexually aroused. Such is the nature of SYMPATHETIC DOMINANCE.
Don’t get me wrong; we all need some ‘hype’ (stress) in our lives. Our response to stress (mechanical, physical, emotional, etc) is what makes us grow and develop both neurologically and physically. Without some degree of stress, life would be rather dull and our brains and bodies would not get the stimulation required to keep them functioning properly and plastic. What we don’t need, however, is dis-stress — ramped-up, over-the-top stress that sends our pulses racing and our blood pressures skyrocketing; often times not because of anything having to do with reality, but from things we are thinking (worrying) about.
George Billman
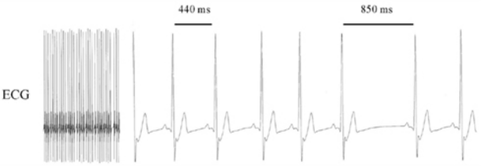
The function of the Autonomic Nervous System (sympathetic -vs- parasympathetic) is measured via something called HRV (Heart Rate Variability). Also known as ‘Cycle Length Variability,’ this simple test has been the standard for determining the state of the Autonomic Nervous System (Parasympathetic -vs- Sympathetic) for decades, both in mainstream medicine and alternative medicine (DR. ROYAL LEE was a big advocate). Heart Rate Variability is simply the variability or difference between the peeks seen on an EKG. Bear in mind that this is not a measurement of a variation on the height of the peeks (intensity of the heart beat), but in the distance between the peeks (frequency).
In other words, Heart Rate Variability measures one’s ability to rapidly (milliseconds) increase or decrease one’s pulse rate in response to stress or changes in environment. Just remember that the faster your body can vary your rate (high variability) is good, indicating you lean toward the parasympathetic side of things. Likewise, a low variability indicates Sympathetic Dominance (see EKG above for example of HRV).
Before we discuss what it will take to solve this all-too-common-but-rarely-talked-about problem of Sympathetic Dominance, let’s take a moment and look at some studies on the subject. For the record, you will frequently see the VAGUS NERVE (Cranial Nerve Ten — always denoted as CN X) mentioned when discussing this topic. The Vagus comes directly off the brain and helps control parasympathetic response in your organs all the way down to the bottom part of the colon. Other areas of parasympathetic nervous control come from the lower brain / brainstem area, as well as the sacrum (tailbone) area. Sympathetic response originates mostly in between these — in the thoracic spine.
Geo-Science International
“In a constantly stressed state, vessels adapt to constriction, becoming muscular and therefore maintaining an extremely narrow diameter, requiring larger amounts of blood to be pumped through them naturally increasing blood pressure. Appetite suppression is a common symptom of sympathetic dominance. Have you ever noticed at work you can go hours on end working on an important pressure packed project without eating much of anything at all? Low libido and arousal are other symptoms of sympathetic dominance. It is not uncommon for older males in very stressful professions to suffer from low testosterone, both men and women can suffer from low estrogen levels which is an antioxidant preventing a number of cardio vascular diseases and atherosclerosis. Due to the seemingly never ending supply of cortisol mobilized glucose, many sympathetic dominant people will retain “stubborn belly fat” as a result. People with stressful, low ranking jobs or stay-at-home parents are at much higher risk of developing health issues related to stress induced sympathetic dominance.”Cherry-picked from Mike Writter’s post on the venerable paleo expert Robb Wolf’s site (Winning The Olimbic Games: Are you on Team Sympathetic or Team Parasympathetic?)
- One of the most fascinating studies I found had to do with BLOOD PRESSURE. If you simply look at the chart above, you’ll notice that blood pressure is increased by your Sympathetic Nervous System. Now listen to this startling admission from the December 2010 issue of the Applied Journal of Physiology (Chronic Activation of the Sympathetic Nervous System is the Dominant Contributor to Systemic Hypertension). “For the past three decades, the renin-angiotensin system has been the major focus in high blood pressure research. The proven value of antihypertensive drugs that block this system has deflected research from other blood pressure-raising systems, including the sympathetic nervous system. Despite this, undeniable evidence exists for the importance of chronic activation of the sympathetic nervous system in the pathogenesis of both experimental and human hypertension.” Interesting, but get a load of this cherry-picked statement showing what actually causes the Sympathetic Dominance that in turn causes hypertension. “The case appears strongest in the experimental overfeeding models of obesity-hypertension. Overfeeding in rats, dogs, and rabbits consistently increases body weight, sympathetic nervous activity, and blood pressure, the activation of the renal sympathetic outflow being particularly prominent.“
- Another extremely fascinating study had to do with DEPRESSION. The January 2015 issue of Progress in Neuropsychopharmacology & Biological Psychiatry (Reactive Heart Rate Variability in Male Patients with First-Episode Major Depressive Disorder) concluded that, “We suggest that in patients with major depressive disorder, autonomic system shifts to sympathetic dominance at rest but toward parasympathetic dominance in response to stress.” This is exactly opposite of what would be considered normal physiology. These people live in a physiologically cranked up internal environment — until they run into a fight-or-flight situation. Only then does their body switch (incorrectly) to parasympathetic control.
- The November 2013 issue of the Oxford Journal of Clinical Endocrinology (Obesity is Associated with an Altered Autonomic Nervous System Response to Nutrient Restriction) concluded that in obese people, “In the obese group, autonomic nervous system tone shifted to sympathetic dominance. After an average weight-loss of 13.8 kg in obese subjects, a trend for sympathetic dominance was found. Our data show that a 48-hour fast leaves autonomic nervous system balance unaltered in lean subjects. In contrast, a 48-hour fast, as well as weight-loss, induces sympathetic dominance in obese humans.” This data certainly makes you want to study FASTING a bit more — particularly skipping a meal.
- Remember THE POST from a couple of weeks ago dealing with the epidemic of video game and porn addiction in young men; hooked to the point they were neither working / going to school, nor entering into fulfilling interpersonal relationships? A study that could easily piggyback on that topic comes from the February 2010 issue of Cardiology in the Young (Associations Between Being Overweight, Variability in Heart Rate, and Well-Being in Young Men). In this study, “data from 786 men with a mean age of 19.4 years (age range from 16 to 24 years) were analyzed in a cross-sectional study: body mass index, sleep duration, sporting activities, psychological well-being, blood pressure, heart rate, and variability in heart rate. Despite the young age of the men in this study, increased values for the body mass index were already associated with a shift in sympathovagal balance trending towards sympathetic dominance. Even in young men, being overweight is associated with increased cardiovascular risk, especially an increased sympathetic and/or lowered cardiovascular tone and increased blood pressure. Our study gives additional motivation for the early prevention and treatment of obesity in childhood and adolescence.” Unfortunately, when the medical community talks about PREVENTION and treatment, they are usually talking about drugs since we have seen that PSA’s and ‘Health Campaigns’ are rather a waste of time and money (HERE).
- Exercise presents an interesting dichotomy when it comes to the Autonomic Nervous System. It is one area that people try and actually induce Sympathetic Dominance for a specific result (a more intense workout or better athletic performance) for a short duration. This is why some people with ADRENAL FATIGUE will continue exercising so hard even though it is contributing to their demise, as it is one of the only things that perks them up and gives them a shot of energy (albeit short-lived). In this 2005 study from the Tohoku Journal of Experimental Medicine we can see this from looking at the study’s title — Music Can Enhance Exercise-Induced Sympathetic Dominancy Assessed by Heart Rate Variability). Why do you think that prior to their games, virtually every athlete you see on TV has his headset on? “Combining music with exercise is therefore not only enjoyable in terms of mood but also may promote physiological excitation and enhance physical activation.“
- In this study on DIABETES as it relates to both NEUROPATHY and EXERCISE, the February 2010 issue of the Tohoku Journal of Experimental Medicine (Increase in the Heart Rate Variability with Deep Breathing in Diabetic Patients After 12-Month Exercise Training) concluded that, “Autonomic neuropathy in diabetes leads to impaired regulation of blood pressure and heart rate variability (HRV), which is due to a shift in cardiac autonomic balance towards sympathetic dominance. Lower HRV has been considered a predictor of cardiac mortality and morbidity. Regular exercise training increases HRV, suggesting a shift in the cardiac sympathovagal balance in favor of parasympathetic dominance in diabetic patients. Long-term physical training may be an effective means to reverse the autonomic dysregulation seen in type 2 diabetes.“
- What about Yoga as exercise, particularly as it relates to CHRONIC LOW BACK PAIN? August’s issue of BMC Complementary and Alternative Medicine (Heart Rate Variability in Chronic Low Back Pain Patients Randomized to Yoga or Standard Care) helped answer that question by concluding that, “Chronic pain can alter the autonomic balance with increased sympathetic activity. The results suggest that yoga practice can shift the autonomic balance towards vagal dominance in patients with chronic low back pain associated with altered alignment of intervertebral discs.” One more thing to add to my FIX YOUR OWN BACK PAIN post. HERE’S another study on HRV and Chronic Pain added after the fact.
- The July issue of the Annals of Neuroscience (Heart Rate Variability in Children with Attention-Deficit/Hyperactivity Disorder: A Pilot Study) revealed that, “Attention deficit / hyperactivity disorder (ADHD) is a common childhood neuropsychiatric disorder. There is autonomic dysfunction in children with ADHD – reduction in overall HRV with sympathovagal imbalance with sympathetic dominance.” With ADHD, we should not be surprised at this result.
- A 2015 issue of the journal COPD (Cardiac Sympathetic Dominance and Systemic Inflammation in COPD) revealed the relationship between Sympathetic Dominance and the extremely common lung problem COPD / Emphysema. “As both autonomic dysfunction and systemic inflammation may contribute to cardiovascular morbidity in COPD, we hypothesized that these may be associated“. More than you knew as we will see in a moment. “The heart rate was significantly higher in patients indicating an overall sympathetic dominance and was inversely correlated with diffusion capacity. Serum IL-6 [a marker for inflammation] was inversely correlated with pNN50, an index of parasympathetic activity… It was concluded that patients with COPD have…. sympathetic dominance. This is associated with decreased lung diffusion capacity and systemic inflammation.” Pay attention as we start getting into this whole “SYSTEMIC INFLAMMATION” thing.
Not surprisingly, other topics of studies I found related to Sympathetic Dominance included, PTSD, REPRODUCTION & SEXUAL AROUSAL, CIGARETTE SMOKE, SPINAL SURGERY, as well as a myriad of others. Here’s the kicker. We should not be surprised at any of this, as there are dozens of studies linking INFLAMMATION itself (as we see in the study above) — the cause of virtually all NON-GENETIC health problems — to decreased Heart Rate Variability
- One year ago this month, Brain Behavior and Immunity (Heart Rate Variability Predicts Levels of Inflammatory Markers: Evidence for the Vagal Anti-Inflammatory Pathway) concluded that, “Evidence from numerous animal models shows that vagal activity regulates inflammatory responses by decreasing cytokine [an inflammatory marker] release. Heart rate variability (HRV) is a reliable index of cardiac vagal regulation and should be inversely related to levels of inflammatory markers. Inflammation is also regulated by sympathetic inputs. We analyzed the relationship between 6 inflammatory markers and HRV. After controlling for sympathetic effects, HRV was found to be inversely associated with fibrinogen, CRP and IL-6. We did not observe consistent sex differences. These results support the existence of the vagal anti-inflammatory pathway and suggest that it has similar effects in men and women.” In other words, high HRV, low inflammation; low HRV, high inflammation. For the record, fibrinogen is one of the intermediates in the whole INFLAMMATION ALWAYS LEADS TO FIBROSIS / SCAR TISSUE scenario.
- January’s issue of Atherosclerosis (Impact of Heart Rate Variability on C-Reactive Protein Concentrations in Japanese Adult Nonsmokers) stated simply that, “Lowered HRV, primarily due to parasympathetic dysfunction, was associated with elevated inflammation, independent of weight, insulin sensitivity, and other related factors.“
- The August issue of Annals of Medicine (Heart Rate, Heart Rate Variability and Inflammatory Biomarkers Among Young and Healthy Adults) came to the conclusion that, “Heart rate, heart rate variability and inflammation are all associated with cardiovascular morbidity and mortality. In this large cohort of young and healthy adults, inflammatory parameters were strongly associated with increased heart rate and decreased heart rate variability, suggesting an important interaction between inflammatory pathways and the autonomic nervous system” Great information, but what about older ‘healthy’ adults?
- Eight years ago this month, the American Heart Journal (Decreased Heart Rate Variability is Associated with Higher Levels of Inflammation in Middle-Aged Men) revealed that, “Many traditional risk factors for coronary artery disease are associated with altered autonomic function. Physical activity, BMI, high-density lipoprotein cholesterol, smoking, depression, and hypertension were directly associated with CRP and IL-6 and inversely associated with one or more HRV variables. C-reactive protein is associated with decreased HRV, even after controlling for traditional coronary artery disease risk factors.” None of this should be surprising except the fact that exercise — particularly too much of it, and particularly hardcore cardio (can anyone say “RUNNING“?) is associated in the scientific literature not only with Sympathetic Dominance and Adrenal Fatigue, but with LEAKY GUT as well.
- As you should be noticing, your body’s ability to maintain homeostasis is easily measured by HRV — its second-by-second ability to regulate heart rate. In other words, Heart Rate Variability is a big deal. Listen to the shocking conclusions from the February 2015 issue of PLoS One (Heart Rate Variability is More Strongly Associated than Inflammatory and other Frequently Used Biomarkers in a Cross Sectional Occupational Sample). “Cross-sectional comprehensive health data of 3947 working adults (avg age 42) was used. Models showed that a global measure of self-rated health is associated with HRV, and that all measures of autonomic nervous system function were significantly more strongly associated with self-rated health than any other biomarker.” This is saying that HRV, as well as things like resting heart and breathing rates are better indicators of your overall health than blood work (biomarkers).
This is why you’ll hear me say time and time again, “Inflammation is Everything“. Unfortunately, I find that very few people can provide a satisfactory DEFINITION OF INFLAMMATION (they usually think it’s synonymous with infection or swelling). Inflammation is a group of chemicals made by your immune system that allows cells to communicate with each other. We need these “biomarkers” (chemicals) in our bodies in order to function and heal properly. The problem is, too much of a good thing is usually a bad thing — in this case a very bad thing. Although THIS PROTOCOL is certainly valid for dealing with most CHRONIC INFLAMMATORY DISEASES or AUTOIMMUNE DISEASES, below are some specific ways to tone down the Sympathetic Dominance and increase your Heart Rate Variability.
WAYS TO CONTROL SYMPATHETIC DOMINANCE, WHILE HELPING
TIP YOUR SYSTEM TOWARDS THE PARASYMPATHTIC SIDE
First, realize that not everyone is Sympathetic Dominant. However, from reading my posts on the subject, it shouldn’t be too difficult to at least have some sort of idea of whether or not you are. And if you’re not quite sure, there are dozens of decent HRV monitors on the market for under two hundred bucks. Secondly, although a non-stressful environment of love and peacefulness is not the cure-all for Sympathetic Dominance, it certainly goes a long way. Thirdly, ever since DR. FRANCES POTTENGER told us to make sure to eat our raw FRUITS & VEGETABLES because they are full of potassium and magnesium that block sympathetic response / heighten parasympathetic response, we’ve had a pretty good idea how to go about tackling this problem via diet. Here are a few others in no particular order.
- LIMIT SCREENS & MEDIA EXPOSURE: Are you getting worked up about the election right now? Don’t. While you certainty have every right to be, doing so isn’t going to change a thing. It’s also important to understand that a great deal of media exposure is purposely designed to deliver an adrenal sympathetic ‘rush’.
- EXERCISE AND DEEP BREATHING: You don’t need to go out and train like a beast. In fact, if you are dealing with chronic health or mental health issues, things like yoga, stretching, Tai Chi, and any number of other low impact forms of exercise are fine.
- EAT THE RIGHT WAY: Avoid foods that initiate sympathetic responses, most of which can be EXTREMELY ADDICTIVE — PROCESSED CARBS and JUNK FOOD, SUGAR, HFCS, caffeine, GLUTEN for some of you (or even some of the NIGHTSHADES pictured above), and any number of others that have the potential to stimulate your adrenals. Beyond this, make sure to eat foods that stimulate parasympathetic response, while limiting sympathetic response. My most frequently recommended diet for regaining and maintaining health? NEED YOU EVEN ASK?
- COMMON SENSE HEALTHY LIFESTYLES: Although most of these are not rocket science, many involve understanding GUT HEALTH. There are large numbers of peer-reviewed studies on quieting techniques such as prayer, meditation, deep breathing, etc.
- AVOID STRESS AND LIVE IN A WORLD OF PEACE AND LOVE: I get it; I sound almost like a 60’s hippy or Bernie supporter here. Just understand that anger, fear, worry, grief, heartache, rejection, suffering, CHRONIC PAIN, powerlessness, hopelessness, insignificance, resentment, jealousy, covetousness, financial burdens, etc, etc, etc) can decimate your health — particularly if that’s what you dwell on. For the record, laughter dampens sympathetic response. One final thought; because sexual arousal is parasympathetic (orgasm itself is sympathetic) make sure to have regular sex and leave lots of time for foreplay.
- MEDICATIONS: Plainly stated, GET OFF AS MANY AS POSSIBLE! Numerous DRUGS have sympathetic side effects because they are specifically designed to stimulate that portion of your Autonomic Nervous System. Some of these SIDE EFFECTS include ANXIETY, restlessness, INSOMNIA, dizziness, HEADACHE, nausea, increased blood pressure, increased heart rate, dry mouth, etc, etc). Bear in mind that the drugs that purposefully cause a parasympathetic response (one of the best known of these would be BETA BLOCKERS) often leave people feeling lethargic, washed out, unmotivated, and sluggish. Dampening the sympathetics is one reason that MARIJUANA and alcohol have such a large following in our chronically stressed out society.
- CHIROPRACTIC ADJUSTMENTS AND / OR FUNCTIONAL NEUROLOGY: For some of you, your Sympathetic Nervous System is stuck in the “on” position and your ADRENAL GLANDS are being perpetually stimulated. Not good. A good FUNCTIONAL NEUROLOGIST can probably help you with this, if you’ve tried everything else. Please realize that CHIROPRACTIC ADJUSTMENTS to the craniosacral portion of your spine stimulate parasympathetic function. As for Tissue Remodeling (especially for CHRONIC NECK ISSUES); it can activate your parasympathetic system as well (HERE).
- OTHERS: If you go to my “SUPER-POST” on Sympathetic Dominance, I show you some real humdingers as far as controlling Sympathetic response is concerned, many of which are ways to stimulate your parasympathetics.
