
CHRONIC NECK PAIN & HEADACHE TESTIMONIALS
CHRONIC NECK PAIN & HEADACHE TESTIMONIALS (Lots of Videos. Give it a Few Seconds to Load) CASSIE MULDER Cassie was seriously injured in a cheer
Mountain View, MO 65548
Call for an appointment
Closed 12:00 - 1:00

CHRONIC NECK PAIN & HEADACHE TESTIMONIALS (Lots of Videos. Give it a Few Seconds to Load) CASSIE MULDER Cassie was seriously injured in a cheer
Chronic Headaches Almost everyone has endured a headache, and has at least some kind of idea of what they are like. There is, however, a

WHAT DOES THE LATEST RESEARCH ON NECK PAIN, HEADACHES, AND WHIPLASH REVEAL? “Neck pain is the most common musculoskeletal pathology second only to low back

AMERICAN HEADACHE SOCIETY NOW RECOMMENDING COMPLIMENTARY TREATMENT FOR CHRONIC HEADACHES IS THE SKY FALLING? Dr. Rebecca Wells is a neurologist at Winston-Salem’s Wake Forest

Back in June a team of Swedish researchers put together a study for the Journal of Pain Research titled Exploring Patients’ Experiences of the Whiplash

SOLUTIONS FOR CHRONIC HEADACHE AND MIGRAINE?THE DAITH Over the past few years I have seen numerous patients with the “Daith” ear piercing (see pic above
A STEP-WISE APPROACH TO SOLVING YOUR CHRONIC HEADACHES AND MIGRAINE HEADACHES The June issue of the journal for pain doctors, Practical Pain Management, carried an

CHRONIC NECK PAIN: TENSION HEADACHES -VS- CERVICOGENIC HEADACHES It’s estimated that about half the adults in the UK experience tension-type headaches once or twice a

MIGRAINE HEADACHES: CHEMICAL, MECHANICAL OR ELECTRICAL? Let me first say that technically speaking, many of the migraines diagnosed as migraines are not really migraines —
CHRONIC NECK PAIN & HEADACHES?THE FIRST STEP TO FINDING A SOLUTION IS RESTORING RANGE OF MOTION “A personal frustration as a clinician and researcher in

BMJ‘s “BEST EVIDENCE” FOR TREATING HEADACHES As many of you know, I not only love what I do, but I love evidence for what I

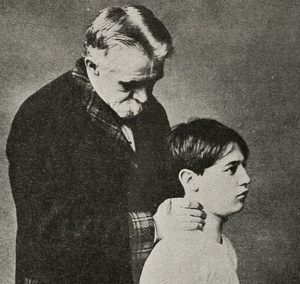
CHILDREN IN PAIN(HEADACHES) “Children and their parents should understand that there are no miracle cures for headaches.” Dr Lawrence Robbins from the article discussed today.

HEADACHES AND CHRONIC NECK PAINCAUSES & SOLUTIONS Wellcome Images #V0008244 “Among chronic pain disorders, pain arising from various structures of the spine constitutes the majority
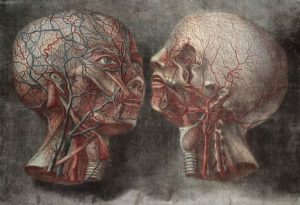
THE RELATIONSHIP BETWEEN CHRONICHEADACHES,SKULL PAIN, AND FACE PAINIS IT ALL THE SAME THING? Wellcome Trust # L0023747 “Headache and facial pain are common complaints in

MIGRAINE HEADACHESAND ADHESED FASCIA Klaus Hausmann – Köln/Deutschland – Pixabay “More than 60 million American adults report experiencing a migraine, and they affect women at

CHRONIC NECK PAINAND CHRONIC HEADACHESTWO COMMON PROBLEMS THAT GO TOGETHER LIKE A HAND IN A GLOVE Kai Kalhh – Hamburg/Deutschland – Pixabay “Headaches account for

THE RELATIONSHIP BETWEEN BLACK MOLD AND MIGRAINE HEADACHES Infrogmation A couple of months ago I had a mother come in with her two young kids.

CHRONIC NECK PAIN AND HEADACHESHOW MANY AMERICANS STRUGGLE WITH THIS COMMON PROBLEM? Vishnu Vijayan – kerala/India – Pixabay Neck Pain and Headaches. Unfortunately, these two

TEENAGERS WITH HEADACHES?MAKE EM PART OF THE OPIOID EPIDEMIC!GIVE THEM DRUGS! Arek Socha – Stockholm/Sweden – Pixabay “Opioids were go-to drugs for teen headache even
HEADACHE OR SKULL PAIN…IS THERE REALLY A DIFFERENCE? Since I can remember, I would infrequently get these sensations in my head, painful, and the only
Enter your name, email address and message in the box below to send us an email. If you’re in the Mountain View area, you can stop in to the office. We’re located in Mountain View at: 1219 South State, Route 17. Or, give us a call at: (417) 934 6337